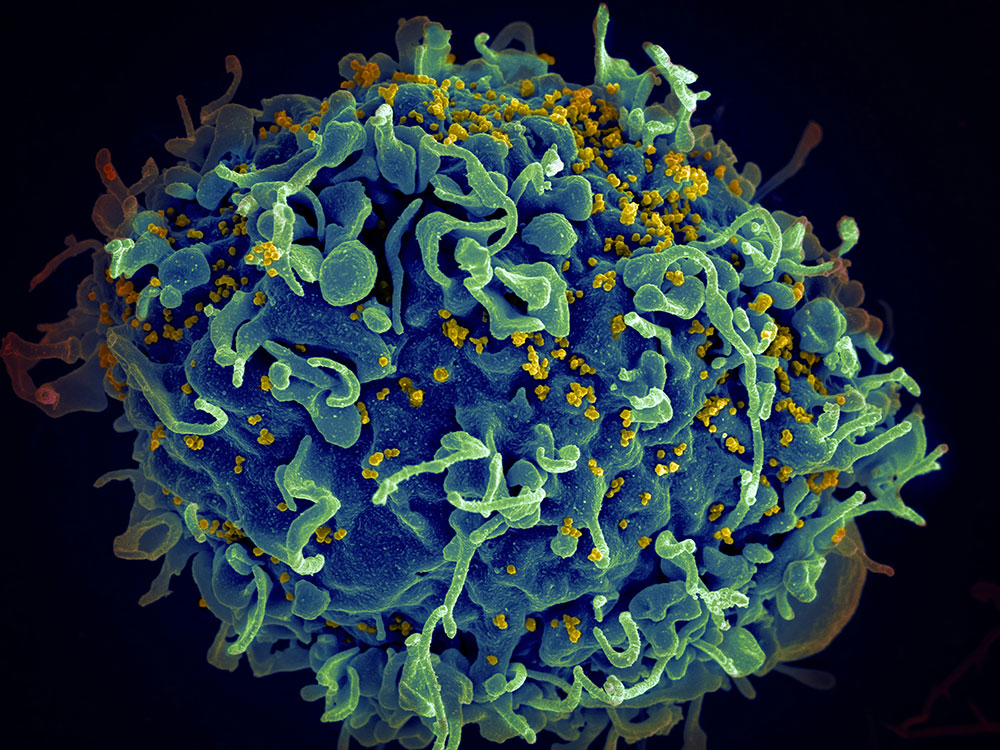
Accurate monitoring of CD4+ T cell counts is vital for evaluating immune health and guiding treatment in people living with Human Immunodeficiency Virus (HIV). Yet conventional tools like flow cytometry, while highly effective, are expensive, complex, and ill-suited for widespread use in remote or resource-limited areas. Many portable alternatives remain constrained by low sensitivity, intricate sample handling, or high operational costs. Optical and fluorescence-based systems, though advanced, further compound these issues with their maintenance and equipment needs. Due to these limitations, there is an urgent need for cost-effective, standalone diagnostic platforms that can be deployed directly at the point of care to ensure timely HIV monitoring.
In a collaborative effort, researchers from the University of Bath and Nanyang Technological University have developed an integrated microfluidic electrochemical biosensor for detecting CD4+ T cells. Their findings (DOI: 10.1038/s41378-025-00893-8), published on April 9, 2025, in Microsystems & Nanoengineering, showcase a polydimethylsiloxane (PDMS)-based chip with gold electrodes that uses impedance-based, label-free sensing. Tailored for low-resource settings, the device enables minimizing handling steps and simplifying sample processing, and delivers results within clinically relevant thresholds. This breakthrough marks an important advance toward enabling real-time HIV diagnostics outside of conventional laboratories.
At the core of the device is a microfluidic chip embedded with gold electrodes, which enables both the functionalization and detection processes to occur on-chip. Anti-CD4 antibodies are immobilized via self-assembled monolayers, ensuring specific binding of target cells. The sensor’s wide dynamic range captures both immunocompromised and healthy CD4+ levels, with a detection limit that can identify advanced immunodeficiency. Compared to traditional bench-top systems, the microfluidic design significantly reduces variation and manual labor, improving reproducibility and making the device well-suited for automation. Specificity tests showed negligible interference from monocytes, neutrophils, and common serum proteins. The sensor can also be paired with a Dean Flow Fractionation chip for upstream cell separation, allowing for a fully modular system that integrates cell isolation, capture, and enumeration—all on a single device.
“Our goal was to develop a user-friendly, affordable diagnostic tool that could extend high-quality HIV monitoring beyond centralized labs,” said Professor. Pedro Estrela, the study’s corresponding author. “By combining electrochemical sensing with microfluidics, we’ve created a platform that is not only accurate and sensitive, but also scalable and compatible with point-of-care use. This technology has the potential to democratize access to HIV diagnostics, especially in regions with limited medical infrastructure.”
Looking ahead, this microfluidic biosensor could serve as a transformative tool for HIV management in underserved regions, replacing bulky laboratory instruments with portable, battery-powered alternatives. Its flexible design supports the integration of automated sample processing and multiplexed detection of other immune markers or pathogens. The next development stages will involve integrating the DFF chip for whole blood testing, clinical validation, and refining user interfaces for field deployment. Ultimately, this technology could lead to robust point-of-care platforms that support early diagnosis, strengthen treatment monitoring, and advance equitable healthcare delivery in global HIV control efforts.